Learning More About Myocarditis And Pericarditis
The recent report of a slightly increased risks of myocarditis or pericarditis in adolescents and young adults following the COVID 19 vaccination have resulted in more interest in this condition.
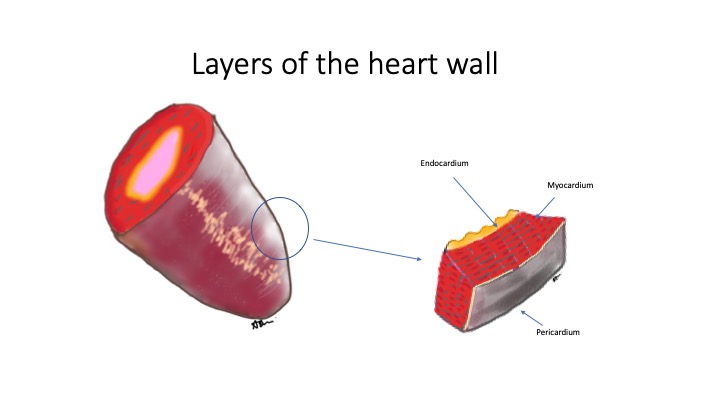
To understand this further, we will need to first learn more about the heart structure.
The walls of the heart chamber consist of 3 layers:
- Endocardium (inner lining of the heart and the flaps that form the heart valves)
- Myocardium (muscle part of the heart responsible for contraction)
- Epicardium (outermost layer of the heart)
The heart is then wrapped by a thin membrane called the pericardium.
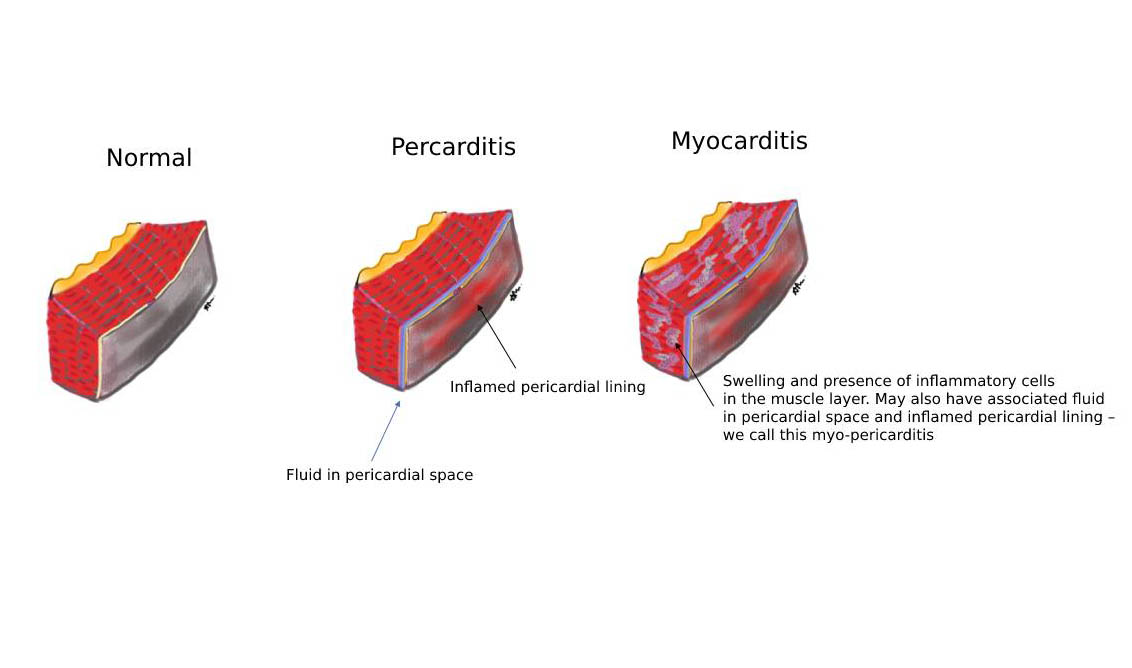
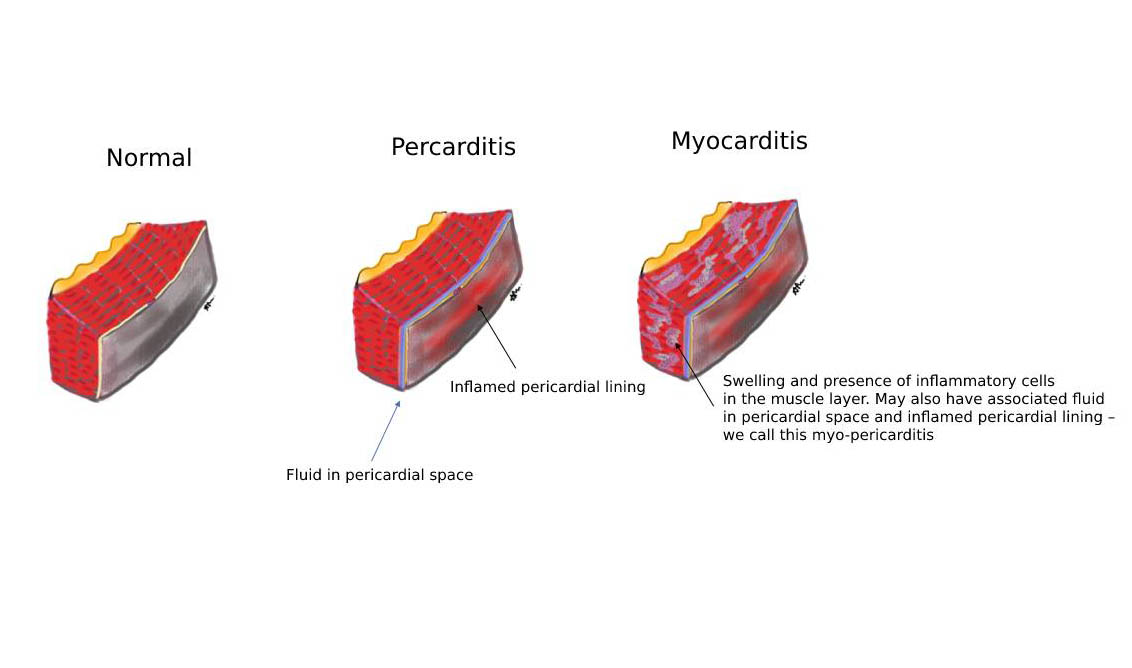
When inflammation occurs in the myocardium – we call this myocarditis. Similarly, when inflammation occurs at the membrane surround the heart (pericardium) we term this pericarditis.
What are the causes of myocarditis/pericarditis?
This can be caused by both infectious (caused by a pathogen or germ) and non-infectious conditions.
Infectious conditions include those caused by viruses, bacteria, fungal or parasitic infections.
Non-infectious conditions include those caused by certain drugs or toxins. Others may be related to a hypersensitivity condition or other medical disorders like celiac disease, collagen vascular disease, thyroid disease, inflammatory bowel disease). Radiation therapy can also cause this.
What are the known rates of occurrence?
In one published study (Global burden of Cardiovascular Disease and Risk Factors study) in 2019 (not related to COVID 19), the rate of myocarditis was 6.1 per 100,000 in men and 4.4 per 100,000 in women aged 35-39 years of age. Mortality rate because of this was about 0.1-0.2 per 100,000.
What are the symptoms of myocarditis?
This can be highly variable:
- Many may be subclinical (no symptoms)
- Some may have associated symptoms of fever, muscle pain fatigue (this could also be from the viral infection itself)
- Chest pain (often vague)
- Fast heartbeat
- Heart failure (this often presents with generally feeling of being unwell, breathless, fast heart rate, dizziness)
- Low blood pressure associated with symptoms of dizziness/faints.
- Sudden death
What are the symptoms of pericarditis?
There are some overlapping symptoms with myocarditis, however, there may be some unique chest pain features which may suggest pericarditis.
This includes pain on taking in a breath or pain which is worsened when a person lies supine and better on leaning forward or sitting up.
It is important to also know that the presentation of myocarditis can be acute occurring within days to weeks (more dramatic symptoms) or chronic which tends to occur over a few months (more gradual and less dramatic symptoms)
How does a cardiologist diagnose this condition?
- A detailed history is needed.
- Physical examination in the clinic
Test which are sometimes ordered (these would be guided by your cardiologist)
Electrocardiogram (ECG) this is especially useful to look at the electrical patterns as well as the rate and rhythm of the heart.
Blood tests
C -reactive protein – a marker of inflammation
Erytrocyte sedimentation rate (ESR) – another marker for inflammation
Full blood count – This allows the doctor to assess the white cell count which can give clues to whether this is related to a viral or bacterial infection. A unique type of myocarditis may be related to high levels of a blood cell call the eosinophils
Cardiac biomarkers such as troponin levels (which are a direct marker of myocardial cell injury)
Chest X- ray to look at the heart size and lung field.
Brain natriuretic peptide – to assess for the possibility of heart failure in some patients.
Imaging tests
Transthoracic echocardiogram – this is a non-invasive ultrasound which allows the cardiologist to look at the heart function, structure, and pericardium. Occasionally fluid may be seen in the pericardial space.
Cardiac magnetic resonance imaging. This test is useful to look at the extent of muscle injury ( it would be able to pick up tissue damage, edema/swelling of muscle tissue or even scar formation after the resolution of the injury)
Invasive testing in some very sick/ severe heart failure patients
Occasionally, an endomyocardial biopsy of the cardiac tissue and assessment of the histology and cells under the microscope is recommended for some patients.
Right heart catheterization may also be done to assess cardiac function in some patients with heart failure.
References:
1: Roth GA, Mensah GA, Johnson CO, Addolorato G, et al. GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020 Dec 22;76(25):2982-3021.